What is CORE Syndrome?
A 45-year-old patient that I have been following for several years, who first came to me due to his chronic recurrent sinusitis, was diagnosed with two underlying risk factors for his disease: immunoglobulin deficiency plus reflux. Once the risk factors were identified, the patient’s sinus symptoms improved significantly with subcutaneous immunoglobulin injections and daily use of a proton pump inhibitor, plus lifestyle changes. Unfortunately, over the past two years, the patient has had an increase in symptoms with both mild sinus congestion and cough due to post nasal drip.
The patient was also complaining of sweats at night, which were not associated with fevers or weight loss. The patient is also an avid runner and was finding it difficult to continue his running regimen based on the cough and an inability to breathe deeply while running.
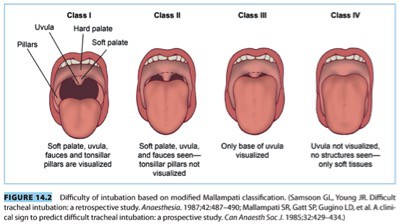
Despite being in excellent shape, there was concern that the patient may have had obstructive sleep apnea. This patient, in particular, did not show any of the typical risk factors associated with obstructive sleep apnea. He was not overweight, did not have a neck circumference over 17 inches and did not carry a significant amount of weight in the chest. All of the above physical attributes are usually associated with obstructive sleep apnea. However, the patient did have macroglossia, in other words, a large tongue which obstructed the patient’s uvula completely. Malampatti scoring is used to help anesthesiologists predict the difficulty there will be to intubate a patient. It has also been a helpful tool in identifying patients at risk of obstructive sleep apnea. The more obstruction there is, the more difficult the intubation. Malampatti scoring ranges from class I to class IV with class IV being the most obstructive. For this individual, he was class IV.
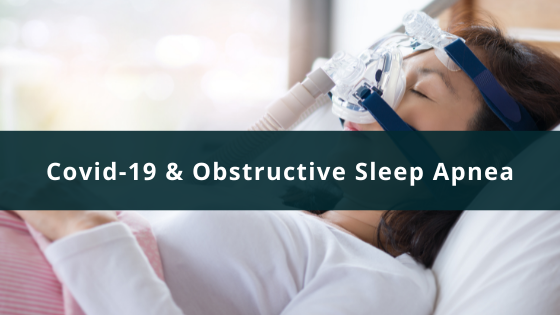
Based on the patient’s history and physical findings, a home sleep study was ordered. The patient did show moderate to severe obstructive sleep apnea with oxygen desaturation into the upper 80s.
The patient was extremely reluctant to try a CPAP to correct the underlying obstructive sleep apnea but was willing to try an oral appliance. The patient was compliant with the oral appliance and did have some improvement. However, his exercise tolerance was not where he had hoped it would be due to the continuation of his chronic cough.
Recently the patient agreed to have a CPAP trial and is currently on a CPAP. Since being on his CPAP, he has noticed a significant improvement in his breathing, especially since there is a lack of a chronic cough at this time. The patient is now making plans to run the 2019 New York City Marathon, as part of a 10 year anniversary with several friends.
This patient has the classic findings associated with a very little known syndrome called CORE syndrome. CORE syndrome stands for chronic cough/asthma, obstructive sleep apnea, rhinosinusitis, and esophageal reflux disease. Some patients have esophageal reflux disease which is associated with their obstructive sleep apnea which then exacerbates both their recurrent chronic sinusitis and chronic cough.
Obstructive sleep apnea can worsen esophageal reflux disease. The best explanation out there concludes that during the apneic event, the individual tries to override the apnea by taking a deep breath during sleep, thereby creating negative pressure inside the chest cavity allowing gastric contents to come back up into the throat, sinuses, and lungs. When this occurs, it aggravates both asthma and sinusitis by creating mucosal damage to both areas.
In this particular individual, despite adhering to medications for his reflux and lifestyle changes, and despite being extremely fit and active, the patient was still experiencing symptoms. It wasn’t until we finally addressed his underlying obstructive sleep apnea with a CPAP, that he was able to see significant improvements.
As in many of these cases, treatment is based on not only identifying underlying risk factors but then realizing that all aspects must be optimally managed. If this does not happen, patients are unable to maximally manage their disease process.