A Look At Enterobacter Sinusitis & GERD
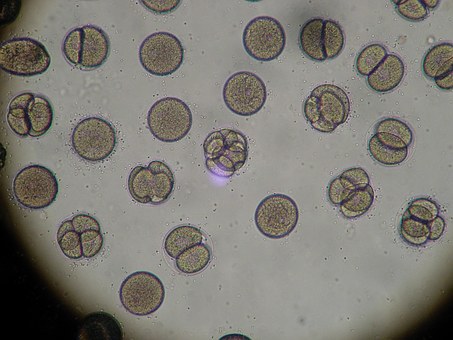
Enterobacter and gram-negative enteric infections have been on the rise for the past three decades. In most instances, infections usually involve the abdomen, bloodstream or the urinary tract. Though seen by clinicians that do extensive work in chronic recurrent sinusitis (CRS) Enterobacter and other gram-negative enteric sinusitis seen in the outpatient setting has been rarely described in the medical literature. The following cases describe the diagnostic process by which three patients were managed with Enterobacter sp sinusitis.
Enterobacter Sinusitis in 48 y/o Female: Case 1
A 48-year-old female with a longstanding history of chronic sinusitis had endoscopic sinus surgery three months prior to evaluation at our facility. Since her surgery, the patient had been treated twice for sinus infections. During her second flare up culture revealed Enterobacter cloacae sensitive to all fluoroquinolones. Despite being treated adequately twice with levofloxacin the patient continued to have recurrent infections.
According to the patient, she believed that the sinus infections post-operatively were worse than before surgery. The patient also stated that issues with recurrent sinusitis did not start until the pregnancy with her third child which was quite large (the baby was 9lbs, 12oz at birth). Since that time the patient admitted to excessive post nasal drip (PND) which was worse in the morning. She did deny symptoms of heartburn.
Pertinent findings on the physical exam were an edematous and erythematous uvula, plus erythema of the oropharynx and postnasal discharge.
Due to the extent of the patient’s infection, it was decided to use intravenous antibiotics, while concomitantly treating underlying reflux with omeprazole and bicarbonate. After 8 weeks the patient was infection free and at the three-month follow-up, the patient had no further recurrence of sinusitis. Also, the patient realized improvement of postnasal drip since being put on Zegerid.
Enterobacter Sinusitis in 38 y/o Male: Case 2
A 38-year-old male with a long-standing history of recurrent bacterial sinusitis was found to be growing Enterobacter from the sinuses which was sensitive and responsive to levofloxacin on multiple occasions. However, the patient was concerned with the fact that despite appropriate therapy his symptoms were recurrent. The patient had also undergone endoscopic surgery twice. At the time of evaluation, he was symptom-free but he realized it was only a matter of time.
The patient denied any symptoms of dyspepsia but did admit to frequent throat clearing due to excessive postnasal drip especially upon waking. Also, the patient admitted to a cough but he denied asthma. Pertinent physical findings included erythema of the uvula and oropharynx. The management plan for this patient was to treat with omeprazole/bicarbonate alone considering the patient did not have an acute infection at the time.
Enterobacter Sinusitis in 71 y/o Female: Case 2
A 71-year-old woman with a long-standing history of recurrent CRS, which has worsened over the last several years, came to our facility being treated for the third time with Enterobacter sinusitis sensitive to Bactrim. According to the patient and her otolaryngologist, this was the patient’s third post-operative infection since surgery was done three months prior to this visit.
Other associated symptoms included SOB, wheezing and increased PND especially in the morning. As with the other two patients, she denied dyspepsia but admitted to recurrent bouts of hoarseness.
Pertinent physical findings included: erythematous and edematous uvula with post nasal secretions noted in the oropharynx. Other pertinent finding included purulent and bloody discharge in the nasal passages bilaterally with edema and erythema of the turbinates.
In this case, the patient completed her course of Bactrim and was initiated on dexlansoprazole 60 mg daily. In the past seven months, the patient has had only one minor flare-up of her CRS and Enterobacter was not cultured.
Discussion:
Gram-negative infections have been on the rise for the past three decades, and nosocomial sinusitis due to E. coli, K. pneumoniae, P. aeruginosa, and Enterobacter species are well described in the literature. In most instances, infections follow manipulation of the urinary, respiratory or gastrointestinal tracts. In the case of nosocomial sinusitis, it usually occurs with nasal intubation or nasogastric tubing.
In the three cases described, the patients’ procedures were outpatient procedures. The literature on gram-negative sinusitis associated with endoscopic surgery has been sparse to date. Recently one study on the subject has been published in Chinese medical literature.
A recent study looked at the clinical correlation between irrigation bottle contamination and post-functional endoscopic sinus surgery. The findings demonstrated that use of an irrigation bottle greater than 1 week increased the risk of contamination with gram-negative enterics. It also concluded that contamination did not result in postoperative infections. However, follow-up concluded at week four post surgery.
The question that was not asked though was what caused the contamination?
In the study again the associated bacteria included: P. aeruginosa, Acinetobacter baumannii, K. pneumonia, E.coli and Enterobacter spp. All of these organisms are associated with the gastrointestinal tract. The origin of the recurrent sinus infections of the patients being described in this paper most likely is gastrointestinal in nature.
It is difficult for many to believe that gastroesophageal reflux (GERD) can affect chronic rhinosinusitis, but GERD has several extra-esophageal manifestations. These include; asthma, chronic cough, and laryngeal disorders along with CRS. In many instances classic symptoms of GERD are absent and the diagnosis is not considered. Also in many of these, treatment of the extra-esophageal manifestations of GERD is less predictable than typical GERD.
In all three cases, underlying GERD was not considered because of the extra-esophageal manifestation and the lack of typical symptoms. In other words, their GERD was “silent” and despite the surgical correction of the patients’ anatomy, they were still symptomatic. In many instances, the patient becomes frustrated and demoralized believing that the recurrent infection is a direct result of the surgery either due to the surgeon, the facility or both.
Many of these patients after a while do not return for follow-up believing this is as good as it gets. They return to their primary care physicians who periodically put the patients on courses of oral antibiotics which continue over months and years, which in turn can lead to further problems with side effects and resistance development. In the above cases, the corner-stone of their therapy was treating the underlying risk factor of GERD, which was silent. In this way, further, necessary but avoidable antibiotics use was not indicated.
In conclusion, by understanding the consequences of silent GERD and the origin of how these sinus infections come about, the clinician will be better armed to assist these difficult patients. In return, the patient can move on with their lives symptom-free and the overuse of necessary antibiotic therapy is avoided which will help address the concern of antibiotic use and increased resistance.
Sources:
[1] Infections due to gram-negative bacteria: an overview, Neu HC, Rev Infect Dis. 1985, Nov-Dec; 7 Suppl 4: S778-82
[2] Chinese medical literature Bacteriological study on chronic sinusitis operated after endoscopic sinus surgery, Yang XH, Li Y, Gao XQ, Chen QM, Li XH, Liu X, Li JD. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2007 Dec 42(12): 904-9. An article in Chinese Abstract only.
[3] Clinical correlation between irrigation bottle contamination and clinical outcomes in post-functional endoscopic sinus surgery patients. Welch KC, Cohen MB, Doghramji, Cohen NA, Chandra RK, Palmer JN, Chiu AG. Am J Rhinol Allergy. 2009 Jul-Aug; 23(4):401-4.
[4] Infectious Diseases: Cohen, Powderly 2nd ed. 2004, Mosby, Chapters 228 and 229. pgs2189-2225.
[5] Prevalence, diagnosis and treatment of extra-esophageal manifestations of GERD, Sugawa T, Fujiwara Y, Tanigawa, Shiba M, Tominaga K, Watanabe T, Oshitani, N Higuchi K, Arakawa T. Nippon Rinsho, 2007, May; 65 (5) 946-50
[6] Extra-esophageal symptoms of GERD, DeValt KR, Cleve Clin J Med. 2003, Nov; Suppl 5: S20-32.
[7] Ibid.