The Role of Anti-fungal Agents
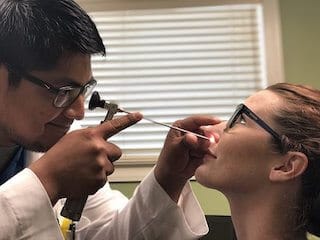
A 39-year-old female presented to my office several weeks ago with a history of recurrent chronic sinusitis. According to the patient, her symptoms of chronic sinusitis were pretty much persistent and that multiple courses of antibiotics would improve her symptoms but, she never would feel well. DNA analysis performed by her otolaryngologist confirmed the diagnosis of allergic fungal sinusitis with Epicoccum nigrum. Prior to the patient’s DNA analysis in addition to antibiotic therapy, the patient also received systemic and topical steroids and the patient was also tried on a combination of topical antibiotics and steroids.
Epicoccum nigrum is considered one of the toxicogenic black molds. Other molds in this category include Alternaria and Pullularia. Toxigenic molds have been associated with a variety of symptoms including both respiratory and neurologic in nature. Epicoccum has been associated with both upper and lower respiratory tract disease and has been associated with allergic fungal sinusitis. Based on this patient’s particular history, she was started on oral ketoconazole 200 mg/day. Within a 10 day period time of starting the ketoconazole, the patient had noticed a significant improvement in her symptomatology much greater than what she had seen with antibiotic therapy. The big question is
Why did the patient improve on antibiotics?
The reason for the improvement on antibiotics is related to the secondary bacterial infections that allergic fungal sinusitis creates. Our sinus cavities are normally colonized with bacteria; however, we are not all walking around with sinus infections. This is because the mucosal lining of our sinus cavities provides an excellent barrier to the bacteria and doesn’t allow the bacteria to get into deeper layers and begin to proliferate.
Infections develop when the mucosal integrity of the sinus cavities is disrupted.
Inflammation is a risk factor for disrupting mucosal integrity. With the inflammation that is seen with allergic fungal sinusitis, disruption of the mucosal lining allows for bacterial proliferation and subsequent infections. This is very similar to what happens when our skin is scraped. Our skin is covered with bacteria, yet the skin acts as an excellent barrier to prevent us from having bacterial infections. If there is damage to the skin and there is a wound, which is not cleaned, we develop an infection. This is basically the same that happens in our sinus cavities. Chronic inflammation allows for the proliferation of bacteria and subsequent infections. Herein lies why the patient experienced some relief with antibiotics.
Unfortunately, in this case, the major underlying risk factor was not being addressed properly. Steroids have long been a major adjunct in treating allergic fungal sinusitis, and there are those who still believe that the treatment of choice for allergic fungal sinusitis is steroids. Steroids, however, only reduce the inflammation and the benefit of steroids is only seen while the patient is on steroid therapy. In many instances, symptoms return after steroids are stopped just like as seen with antibiotics.
There are those patients that have been diagnosed with allergic fungal sinusitis that do too well with topical steroid therapy. However, the majority of these patients have recurrent symptoms despite steroid therapy.
The delivery method for this therapy can be topical, orally or intravenously. The delivery method should be based on the severity of disease where the intravenous use of antifungals should be limited to patients with extensive or invasive disease. Once the patient is stable a maintenance regimen needs to be tailored to the individual patient.
Allergic fungal sinusitis, in my opinion, is very much underdiagnosed here in the United States. This is because up until the time of DNA analysis growing fungus by routine culture technique was extremely unreliable. DNA analysis will allow us to identify allergic fungal sinusitis in patients with chronic sinusitis that has been refractory to conventional therapy and allow clinicians to treat these more difficult cases better.