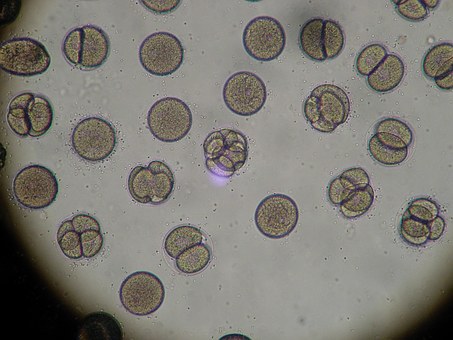
The Gram-positive aerobe Staphylococcus aureus (S. aureus) is one of the most important pathogens, as it causes a variety of infections in both pediatric and adult patients, from generally minor skin infections such as boils and cellulitis to life-threatening infections such as endocarditis and sepsis (1,2). In addition, because of its virulence and the widespread use of broad-spectrum antibiotics. S. aureus has developed resistance to many oral, topical, and parenteral antibiotics. Methicillin-resistant S. aureus (MRSA) has become especially important in recent years because of its increasing prevalence in patients with acute and chronic sinusitis, (3,4), as well as, its presence in the nasal mucosa of normal individuals (5). The normal, healthy sinus is a nonsterile environment colonized with aerobic and anaerobic bacteria, including S. aureus (6,7). At any given time, S. aureus occupies the anterior nares of approximately one-third of the human population (2,8,9).
Chronic sinusitis is a poorly understood disease with many pathophysiologic mechanisms (2,10). In general, it is characterized by chronic mucosal inflammation, which is associated with ciliary dysfunction and resulting mucostasis and bacterial overgrowth (2).
Little is known about the role of MRSA in sinonasal infection and its treatment. Management of sinonasal infection caused by MRSA usually consists of a combination of oral and topical antibiotics for 1-2 weeks. Oral antibiotic choices are guided by susceptibility data but usually include trimethoprim/sulfamethoxazole or clindamycin. Intravenous (IV) antibiotics are limited to severe infections, as their efficacy in sinusitis is unclear, and they are usually associated with more adverse events (2). We describe two patients with MRSA sinusitis who failed oral antibiotics but were successfully treated with IV antibiotics.
Case #1
A 43-year-old male with a history of chronic sinusitis underwent endoscopic sinus surgery, septoplasty, and turbinate reduction in December 2008. Approximately 1.5 weeks after surgery, he complained of nasal congestion with epistaxis. After conservative measures, including nasal suctioning, failed, he was empirically started on amoxicillin/clavulanic acid 875/125 mg twice daily. Bilateral nasoendoscopy revealed intense inflammation and generalized oozing in the middle and inferior turbinates. Surgical debridement followed by hemostasis was successfully accomplished. Nasal swab cultures were positive for MRSA, which was sensitive to trimethoprim/sulfamethoxazole. Amoxicillin/clavulanic acid was discontinued, and the patient was started on trimethoprim/sulfamethoxazole 160/800 mg twice daily.
After 2 weeks, he was still symptomatic, with significant purulent material noted bilaterally in the maxillary sinuses. Repeat cultures remained positive for MRSA, which was shown to be sensitive to clindamycin, gentamicin, linezolid, rifampin, tetracycline, trimethoprim/sulfamethoxazole, and vancomycin but resistant to ciprofloxacin, erythromycin, levofloxacin, oxacillin, and penicillin.
The patient, a triathlete who was training for an event, was referred to our care in February 2009. Because swimming was a substantial part of the practice and competition, we were concerned about the possibility of a polymicrobial infection with Gram-negative enteric bacteria. Therefore, based on clinical experience, we initiated treatment with daptomycin 500 mg (6.7 mg/kg) IV once daily in combination with ertapenem 1 g IV once daily. The patient’s progress was documented during weekly dressing changes. Significant improvement with clear sinuses and normal mucosa was observed in sequential endoscopies during the 6 weeks he was on IV antibiotics. The patient tolerated IV antibiotics well.
Case #2
An 82-year-old woman with a long-standing history of chronic sinusitis was referred to our care for further evaluation of complaints of nasal congestion and postnasal drip. Her medical history revealed that she had undergone two endoscopic sinus surgeries a few years earlier. The patient was evaluated, and an endoscopy was performed, which showed mucopurulent discharge and crusting in the left maxillary sinus. The patient was started empirically on levofloxacin 500 mg orally once daily.
Results of the nasal cultures revealed MRSA, which was sensitive to gentamicin, linezolid, rifampin, tetracycline, trimethoprim/sulfamethoxazole, and vancomycin but resistant to levofloxacin as well as ciprofloxacin, clindamycin, erythromycin, oxacillin, and penicillin. Levofloxacin was discontinued, and trimethoprim/sulfamethoxazole 160/800 mg twice daily was started. After 30 days of treatment, the patient was re-examined. Nasal cultures remained positive for MRSA.
The patient was started on daptomycin 4 mg/kg IV once daily for 6 weeks. She tolerated IV antibiotics well. Follow-up endoscopies revealed that she was infection-free, with normal mucosa and no purulent discharge. In addition, MRSA could not be cultured.
Discussion
The prevalence of sinonasal MRSA appears to be increasing, and many unanswered questions remain regarding its role in sinonasal infection and its treatment. Oral antibiotics have been a mainstay of therapy, but not much is known about their penetration into the nasal tissues. While some oral antibiotics have good bioavailability in healthy adults, oral absorption might be altered in older individuals or as a result of drug interactions. Oral absorption of trimethoprim/sulfamethoxazole is good in older adults, as the total area under the curve (AUC) is higher in older than younger adults following a single dose (11). However, the extent of penetration of trimethoprim-sulfamethoxazole into the normal or inflamed nasal mucosa is unknown. It is possible that the concentration of trimethoprim-sulfamethoxazole achieved in the nasal mucosa in our two patients may have been inadequate for the MRSA isolates despite in vitro susceptibility.
We believe this is the first report concerning the use of daptomycin in chronic MRSA sinusitis. Daptomycin is a lipopeptide antibacterial agent with good activity against many Gram-positive pathogens, including MRSA. Daptomycin is indicated for the management of complicated skin and skin structure infections caused by susceptible Gram-positive organisms, including MRSA (12), as well as, methicillin-susceptible and methicillin-resistant S. aureus bloodstream infections, including those with right-sided infective endocarditis (13,14).
In addition to its activity against MRSA, the drug’s pharmacokinetics makes it a good choice for sinusitis infections. Daptomycin penetrates inflammatory blister fluid moderately well, achieving an AUC of 68% relative to plasma. In addition, the maximum concentration in inflammatory fluid was observed to be 28 µg/mL (15), which is several-fold higher than the 90% minimum inhibitory concentration typically observed for MRSA. Daptomycin also penetrates interstitial soft tissue fluid well, achieving an AUC relative to plasma of 93% in subjects with diabetes and 74% in healthy subjects following a single 4 mg/kg IV dose (16).
Although our results should be viewed as preliminary, the success we observed with daptomycin is encouraging, especially given the increasing concerns with MRSA infection.
References
1. Plata K, Rosato AE, Wegrzyn G. Staphylococcus aureus as an infectious agent: overview of biochemistry and molecular genetics of its pathogenicity. Acta Biochimica Polonica 2009;56:1–16.
2. Becker SS, Russell PT, Duncavage JA, Creech CB. Current issues in the management of sinonasal methicillin-resistant Staphylococcus aureus. Curr Opin Otolaryngol Head Neck Surg 2009;17:2–5.
3. Brook I, Foote PA, Hausfeld JN. Increase in the frequency of recovery of methicillin-resistant Staphylococcus aureus in acute and chronic maxillary sinusitis. J Med Microbiol 2008;57:1015–7.
4. Manarey CRA, Anand VK, Huang C. Incidence of methicillin-resistant Staphylococcus aureus causing chronic rhinosinusitis. Laryngoscope 2004;114:939–41.
5. Kuehnert MJ, Kruszon-Moron D, Hill HA, McQuillan G, McAllister SK, Fosheim G, et al. Prevalence of Staphylococcus aureus nasal colonization in the United States, 2001–2002. J Infect Dis 2006;193:172–9.
6. Al-Shemari H, Abou-Hamad W, Libman M, Desrosiers M. Bacteriology of the sinus cavities of asymptomatic individuals after endoscopic sinus surgery. J Otolaryngol 2007;36:43–8.
7. Abou-Hamad W, Matar N, Elias M, Nasr M, Sarkis-Karam D, Hokayem N, et al. Bacterial flora in normal adult maxillary sinuses. Am J Rhinol Allergy 2009;23:261–3.
8. Kluytmans J, van Belkum A, Verbrugh H. Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev 1997;10:505–20.
9. Nouwen JL, Ott A, Kluytmans-Vandenbergh MFQ, Boelens HA, Hofman A, van Belkum A, et al. Predicting the Staphylococcus aureus nasal carrier state: derivation and validation of a “culture rule.” Clin Infect Dis 2004;39:806–11.
10. Bhattacharyya N. The role of infection in chronic rhinosinusitis. Curr Allergy Asthma Rep 2002;2:500–6.
11. Varoquaux O, Lajoie D, Gobert C, Gobert C, Cordonnier P, Ducreuzet C, et al. Pharmacokinetics of the trimethoprim-sulphamethoxazole combination in the elderly. Br J Clin Pharmacol 1985;20:575–81.
12. Arbeit RD, Maki D, Tally FP, Campanaro E, Eisenstein BI; Daptomycin 98-01 and 99-01 Investigators. The safety and efficacy of daptomycin for the treatment of complicated skin and skin-structure infections. Clin Infect Dis 2004;38:1673–81.
13. Rhem SJ, Boucher H, Levine D, Campion M, Eisenstein BI, Vigliani GA, et al. Daptomycin versus vancomycin plus gentamicin for treatment of bacteraemia and endocarditis due to Staphylococcus aureus: subset analysis of patients infected with methicillin-resistant isolates. J Antimicrob Chemother 2008;61:1413–21.
14. Cubicin [prescribing information]. Lexington, MA: Cubist Pharmaceuticals, Inc.; August 2008.
15. Wise R, Gee T, Andrews JM, Dvorchik B, Marshall G. Pharmacokinetics and inflammatory fluid penetration of intravenous daptomycin in volunteers. Antimicrob Agents Chemother 2002;46:31–3.
16. Kim A, Suecof LA, Sutherland CA, Gao L, Kuti JL, Nicolau DP. In vivo microdialysis study of the penetration of daptomycin into soft tissues in diabetic versus healthy volunteers. Antimicrob Agents Chemother 2008;52:3941–6.