Tools to Create a Better Diagnosis for Prostatitis
Chronic prostatitis is divided into two major categories; chronic bacterial prostatitis and chronic non-bacterial prostatitis. According to the literature, chronic bacterial prostatitis is a rare condition, and that bacteria is found in only 5% of the patients with symptoms of chronic prostatitis. Antibiotic therapy is usually a fluoroquinolone like Cipro or Levaquin. Another antibiotic used in chronic bacterial prostatitis is Bactrim. This is based on what is usually cultured from the prostatic secretions which are mostly gram-negative enteric, such as E. coli and Enterobacter. If there is no response to antibiotic therapy, then muscle relaxers or alpha-blockers are recommended for symptomatic relief.
Unfortunately, as with other chronic infections, the true pathogens may not be identified because they are too fastidious to grow on routine culture. The question then has to be asked, maybe it is more than 5% of these symptomatic patients that have a bacterial etiology to their chronic prostatitis?
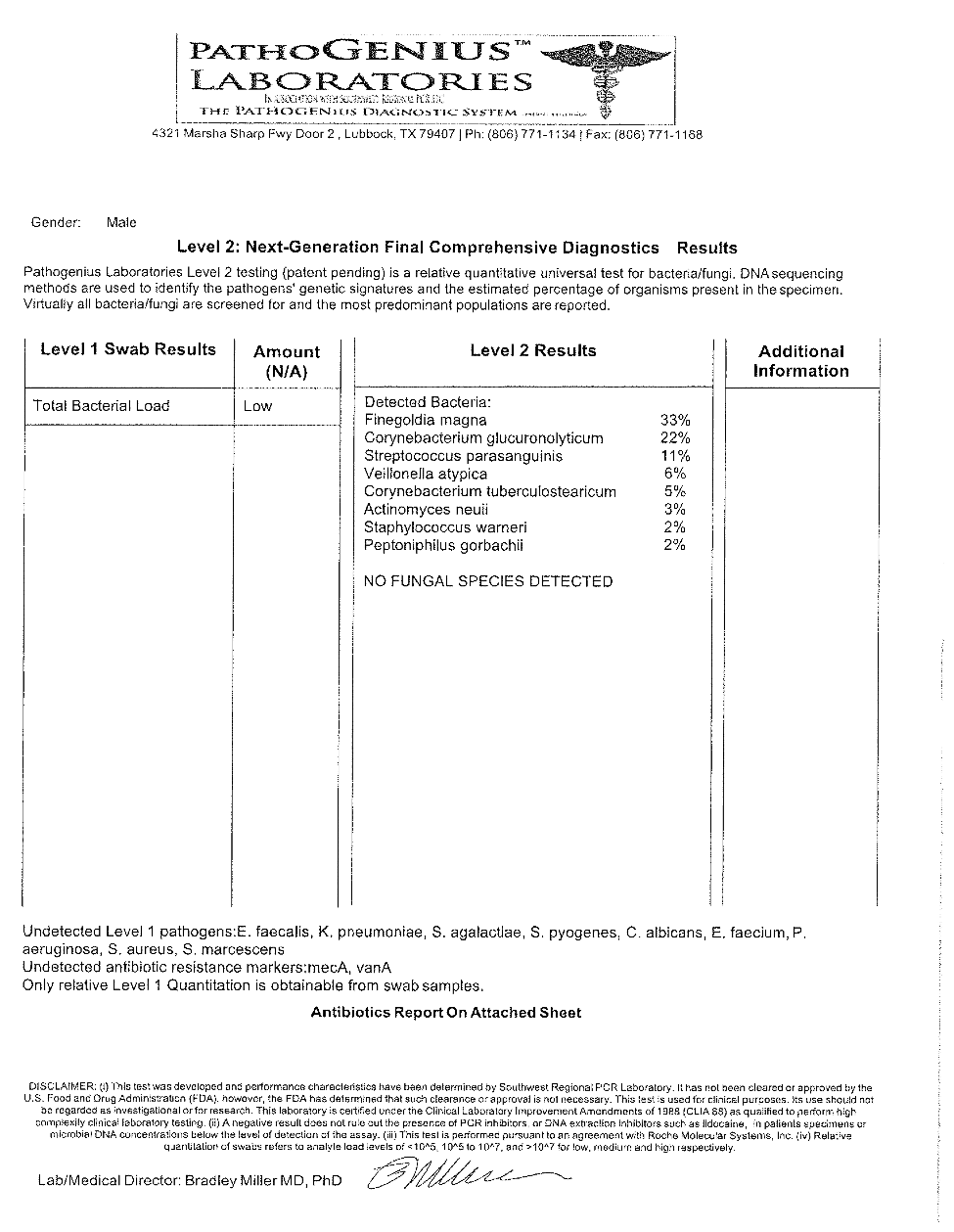
Below is a case of such a patient.
A 55-year-old gentleman had symptoms of chronic prostatitis for over a year and had been to four different urologists and had 25 routine cultures done, all of which were found to be “no growth.” However, DNA analysis revealed the following results:
The patient had been tried on multiple courses of various antibiotics that covered gram negative enterics, but as is seen from the DNA analysis, the bacterial make-up were anaerobes, which do not grow well on media tailored to look for typical organisms associated with urinary problems, which happen to be gram negative enterics. Once the patient was put on oral clindamycin, his symptoms were alleviated. What needs to be remembered is that prostate infections come from the GI tract and that there are more than organisms such as E. coli and Eneterobacter in the GI tract. The GI tract is loaded with anaerobes, and in some instances, the bacterial etiology for chronic prostatitis maybe anaerobic in nature and will not respond to antibiotics like Cipro or Bactrim, which do not cover anaerobes at all and will not culture on routine bacterial media.
Over the years, I have seen several patients with chronic prostatitis who were culture-negative and these patients become frustrated when we, as clinicians, cannot help them. Often these patients are dismissed as kooks or hypochondriacs. It may well be that there is an organic basis to their symptoms and it is bacterial, it’s just that we did not have the tools such as DNA analysis until recently. It is my belief that saying only 5% of all cases of chronic prostatitis have a bacterial etiology is a gross underestimation and that DNA analysis will help in providing a better understanding of the bacterial makeup of chronic prostatitis, and provide more treatment options for patients.